Updated December 15, 2023
Table of contents:
- Who can sign up
- Patient experience
- Patient journey
- Patient charts & encounter notes
- Semi-urgent issues & hand-offs
- Call groups
- Hours
- Things to think about
- Clinic phone system set up
Sign up now to use the after hours care service with your patients. If you need training materials for using the service with your patients, please contact AHCP@doctorsofbc.ca or ahcp.hlbc.admin@gov.bc.ca.
| Click here to sign up |
Who can sign up
-
Family physicians who are members of one of the following divisions of family practice and longitudinal nurse practitioners who are within the geographic boundaries of the following divisions of family practice can sign up to use the after hours service with their patients:
-
Langley Division of Family Practice
-
South Okanagan Similkameen Division of Family Practice
-
South Island Division of Family Practice
-
Thompson Region Division of Family Practice
-
Victoria Division of Family Practice
-
-
Longitudinal nurse practitioners who are within the geographic boundaries of the divisions of family practice listed above can sign up to use the after hours service with their patients.
-
Family physicians who are members of one of the above divisions of family practice can also sign up to staff the service.
-
Physicians and nurse practitioners can sign up individually to use the After Hours Care Service with their longitudinal patients; not everyone in your clinic has to also sign up. However, this might affect your patient-facing messaging or workflows. For example, your voicemail might have to say "Patients of Dr. A or Dr. B, press 1 for care after hours. Patients of Dr. C or nurse practitioner D, press 2."
-
During the pilot, we don’t anticipate that everyone who signs up to use the service for their patients will be required to staff the service. Rather, we’re trying to get a smaller group so that we can simplify training and collect regular feedback about how things are evolving.
-
If it's determined that the service will not extend beyond the pilot, then 60-days notice will be provided to community physicians and nurse practitioners to give them time to restart their call groups.
Patient experience
-
Your patients will either call your existing after hours number and be seamlessly transferred to the after hours service, or your website/voicemail message will give them a number to call for after hours care.
-
A navigator will answer patient calls and ask what assistance they're looking for. The navigator will handle administrative inquiries as appropriate.
-
If the patient has symptoms, then a trained RN will triage the patient.
-
Obvious emergencies will be directed to call 911 or head to the ER.
-
Urgent but non life-threatening issues that fall within the service scope will be transferred to a virtual consult support who will set up a chart (if one doesn’t already exist) and indicate that the after hours clinician will call them back. The caller’s information/chief complaint will be added to a queue, and their chart populated with the triage note.
-
Patient encounters will happen as telephone calls, which are the most common and available technology. Due to the short time frame, the pilot is designed to be low-barrier for quick implementation. The HEiDi service found that a phone call is sufficient most of the time, and the service only uses Zoom occasionally for video calls with patients.
-
FPSC's After Hours Care Program service is not set up to provide crisis or other types of counselling. Patients will be redirected as appropriate to crisis lines, other provincial/community mental health supports, or to follow up with their family physician. If medication advice is required, a patient call may be connected with a pharmacist or to the After Hours Care Program family physician as appropriate.
Patient journey
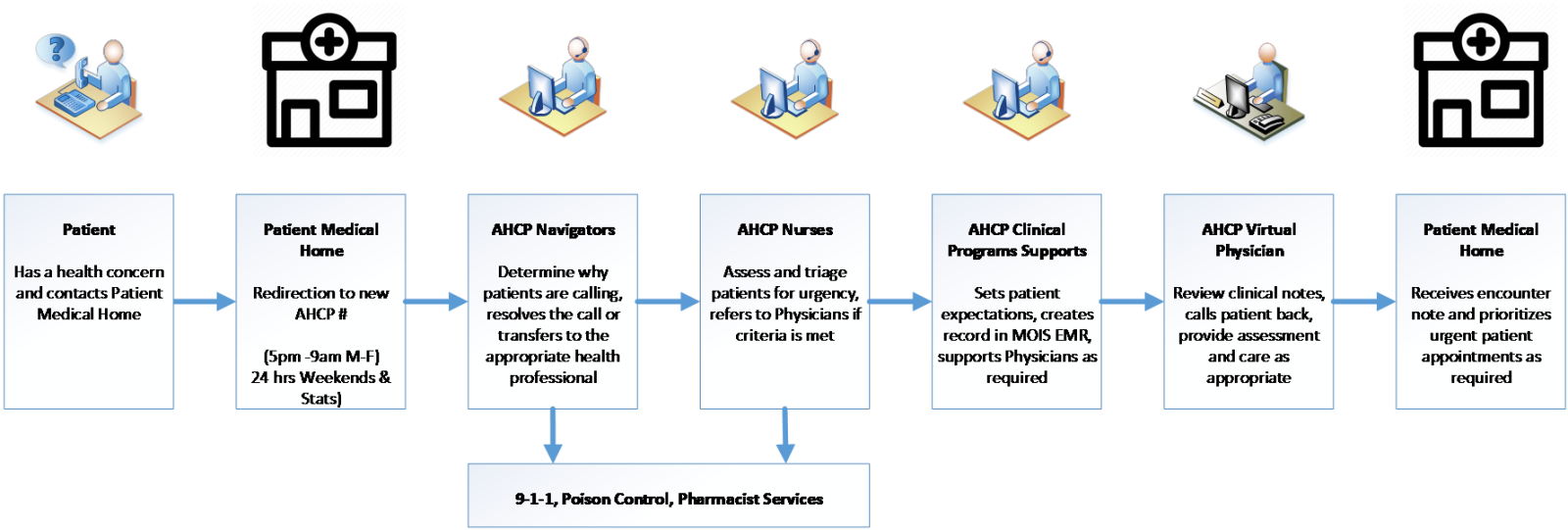
This image shows the patient journey with the After Hours Care program, and the team members involved along the way.
If you have any questions, please contact AHCP@doctorsofbc.ca.
Patient charts & encounter notes
-
While currently there isn't the ability to access a patient’s cumulative health record from community, physicians working the After Hours Care Program service will have access to CareConnect and PharmaNet—more than many on-call doctors currently have.
-
The physician handling the call will be able to look up anything necessary in Care Connect/PharmaNet before calling the patient.
-
After the encounter is finished, a copy of the encounter note will be uploaded to Care Connect and also faxed to the MRP/patient medical home (PMH).
-
If urgent (within 48 hours) follow-up with the MRP is thought to be necessary, then the MRP will receive a phone call from the service in the morning (i.e., between 8:00 – 9:00 a.m. Whether to accept the recommendation from the service about any follow-up is up to the MRP/PMH.
-
The patient chart is owned by HealthLink BC, which has responsibility of keeping records as per the requirements of the College of Physicians and Surgeons of British Columbia. The patient's MRP (most responsible provider) will also have a copy of the encounter note for the patient chart. Should an issue arise and the physician who provided care requires access to a chart in the future, that will be made available.
-
If the After Hours Care Program triage nurse is able to manage the issue, or sends the patient directly to ER, there will not be an encounter note sent to the patient's MRP. While this had been our original goal, the technical implementation of this is still in development and won't be available during the pilot.
Semi-urgent issues & hand-offs
-
When the physician staffing the service deems a patient’s issue to require attention from you within 3 business days, you will be contacted via a phone call to your mobile number. This call will be made by a physician staffing the service the morning following your patient’s call to the service, most likely between 8:00 and 9:00 a.m.
-
If the physician from the service is unable to reach you they will leave a voice message, with a return number. They will also attempt to reach your office to determine how best to reach you. If they are ultimately unable to get a hold of you, they may direct the patient to go to the ER or a local walk-in clinic or UPCC.
-
Ensure you are reasonably able to see patients who need semi-urgent follow-up: While the method should be whatever works best for you, part of using the service is that you will do your best to see patients quickly when semi-urgent follow-up is recommended by the physician staffing the service. This could mean making a couple of rapid-access slots available each week for follow-up on after hours encounters.
Call groups
-
Existing call groups can choose whether or not to participate in the after-hours care service. Joining the service is entirely optional. If not everyone in an existing call group decides to participate, then the group will have to decide how to ensure care continues during the pilot period. Of note, the volume of calls the group receives should decrease, if some members start directing patients to the After Hours Care Program.
-
During the pilot, only calls from attached patients will be accepted—not from facilities or from unattached patients. In addition, if your call group provides care to maternity, palliative or other services, your group will still need to continue those. While FPSC's After Hours Care Program will accept a call from a patient with first trimester bleeding (for example), some calls may be referred to a specialized call group in your community if necessary.
Hours
-
The After Hours Care Program service operates weekdays between 5:00 p.m. -- 9:00 a.m., and 24-hours on weekends and statutory holidays.
- If your office is closed outside of these times, then during the pilot, you'll need to arrange for alternative care as per the College of Physicians and Surgeons of BC requirements.
Things to think about when using the service
This document shares considerations for getting ready to use the after hours service. It is intended to support you in setting up for a successful pilot for both you and your patients.
Clinic phone system set up
Depending on your phone system set up, you will require different logistical and patient messaging modifications. This document covers the five most common clinic phone system set up scenarios.
