Updated September 21, 2023
Table of contents:
- Not your traditional call service
- Patient journey
- Who can staff the service
- Compensation
- Shifts
- Scheduling
- Existing call groups
- Onboarding, training, and support
- Patient encounters
- Patient charts
- Semi-urgent issues
- Unattached patients
You can sign up now to staff the service and to use the service with your patients. The pilot will launch September 19, 2023. Contracts were emailed the week of July 31st to physicians who've already signed up to staff the service. If you need training materials for working the service or using it with your patients, please contact AHCP@doctorsofbc.ca or ahcp.hlbc.admin@gov.bc.ca.
If you're interested in staffing the service or using it with your patients, you can still join! Sign up by clicking this button and completing a short webform.
| Click here to sign up |
The After Hours Care Program is unlike traditional family medicine call. In the Program, family physicians are paid hourly to be available to answer calls. Staffing the service means sitting at the computer, with EMR, CareConnect, and PharmaNet open, monitoring a queue of patients who are waiting to be called back by a physician.
Not your traditional call service
When we talk about staffing the After Hours Care service, many physicians confuse it with traditional "call". Here's a summary of how After Hours Care differs from call:
| Aspect | Traditional call | After Hours Care |
|---|---|---|
| Purpose |
|
|
| Staffed |
|
|
| Shift duration |
|
|
| Availability of on-call physician |
|
|
| Compensation |
|
|
| Call documentation |
|
|
| Billing |
|
|
| Call volume |
|
|
| Main complaints |
|
|
Patient journey
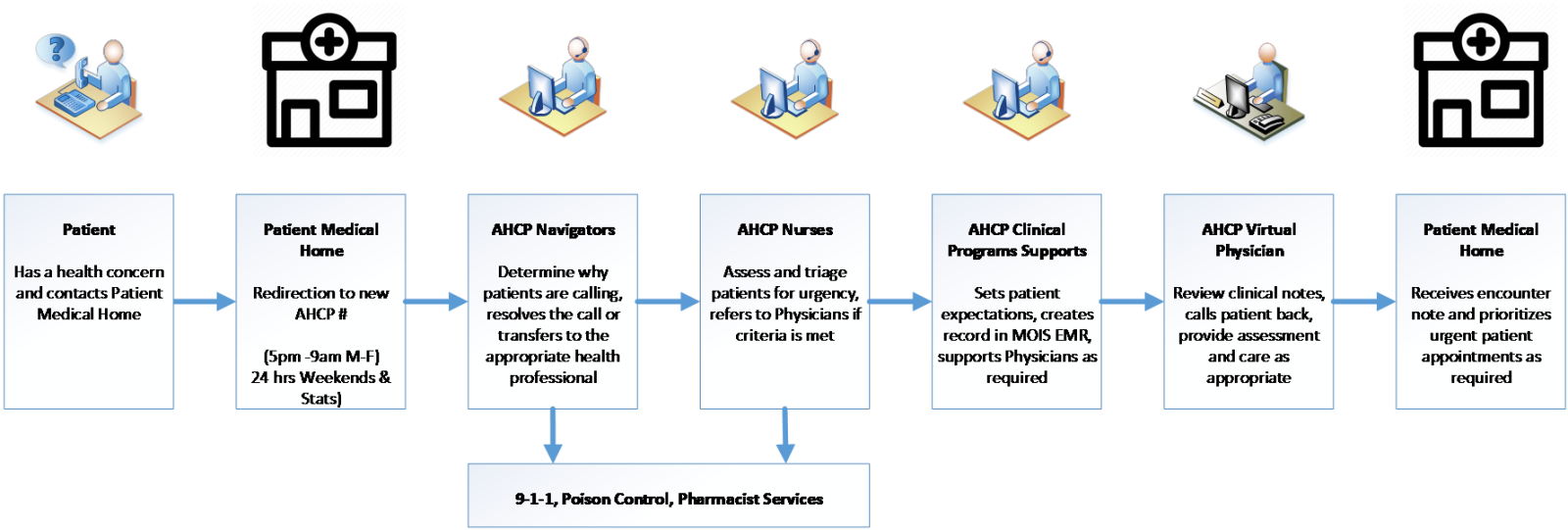
This image shows the patient journey with the After Hours Care program, and the team members involved along the way.
If you have any questions, please contact AHCP@doctorsofbc.ca.
Who can staff the service
-
Family physicians who are members of one of the following divisions of family practice can sign up to use the after hours service with their patients and to staff the service:
-
Langley Division of Family Practice
-
South Okanagan Similkameen Division of Family Practice
-
South Island Division of Family Practice
-
Thompson Region Division of Family Practice
-
Victoria Division of Family Practice
-
-
Longitudinal nurse practitioners who are within the geographic boundaries of the divisions of family practice listed above can sign up to use the after hours service with their patients.
Compensation
-
Family physicians staffing FPSC's After Hours Care Program will be paid through an hourly physician group contract with the Ministry of Health. The Ministry's funding envelope complies with the Physician Master Agreement. Physicians won't need to bill for patient calls. Encounter reporting will be provided to the Ministry of Health.
-
The Physician Group sets the actual compensation rates to drive desired service delivery, recognizing that:
-
The service is compensating for time during each shift and not volume of calls. (While there is no minimum, the maximum number of calls will be 3–5 calls per hour based on how long it actually takes to address those calls and chart.)
-
As this is an extension of the work of longitudinal family physicians, compensation must be consistent with and in consideration of other available opportunities such as working in-clinic, as a hospitalist, or at a UPCC.
-
The service is offered during less desirable times to work.
-
-
The Physician Group provided hourly compensation rates during the June 21 & 22, 2023 introductory webinars to the After Hours Care Program pilot. If you have any questions about compensation, please email ahcp@doctorsofbc.ca.
Shifts
-
The expectation is that in return for hourly compensation, you will be working for the duration of your shift, which involves monitoring the EMR queue of patients and calling back as required. Logging into the EMR for the duration of the shift to monitor patient notifications is required for your review and response to patients.
-
We're asking people who sign up to work the service to sign up for a minimum of 3 shifts (9 hours) per month (split fairly between evening, overnight and early morning) so they don't need to repeat training on how the service works.
-
Each shift is approximately 3-4.5 hours depending on the time of day and the day of the week:
-
4:30 p.m. – 8:00 p.m.
-
8:00 p.m. – 11:00 p.m.
-
11:00 p.m. – 3:00 a.m.
-
3:00 a.m. – 6:00 a.m.
-
6:00 a.m. – 9:00 a.m.
-
-
The shifts are short (3-4.5 hours) so that they shouldn't adversely affect the following day's clinic hours.
-
On weekdays, the first shift starts 30-minutes before the service opens to calls. This allows dedicated time for the service to follow up on labs or other orders.
-
Physicians will be able to sign up for consecutive shifts (e.g., 11:00 p.m.–6:00 a.m. if that is more convenient for scheduling.
-
Physicians staffing the service will likely be limited to a maximum number of shifts per month, depending on recruitment.
Scheduling
-
For the pilot, we are leveraging HealthLink BC's scheduling software for the HEiDi service. This software allows physicians to indicate their overall availability, and then it automatically creates a balanced schedule.
-
During the first few months of the pilot, individuals may be able to sign up for shifts first come, first served—in order to avoid delays in producing the first schedule; this will depend on the number of registrations.
-
Once assigned, shifts can be switched via the scheduling system.
-
If a physician is scheduled to work but has a last-minute illness, then the service team will help with trying to locate a replacement.
Existing call groups
-
While you're simultaneously on call for another group, you're unable to staff the FPSC After Hours Care Program's service.
-
If you're part of a maternity, long-term care, palliative care or in-patient care after hours group, you'll need to continue with your group as these are considered out of scope for the After Hours Care Program's service during the pilot.
-
If you're part of a longitudinal after hours group, then you are welcome to use this service; however, if not everyone in your after hours group decides the same, then you might need to continue to staff your existing after hours group even though your patients aren't using it. As there should be fewer patients using your existing after hours group, the volumes should decrease. This does mean that there should be fewer patients using your existing after hours group, so volumes should decrease. Once the service pilot is deemed successful, then your existing after hours group may wish to switch over to this after hours service entirely.
Onboarding, training, and support
-
Compensated training will be provided as part of the onboarding process.
-
Access to CareConnect, Pharmanet, and HealthLink BC's EMR (MOIS), will be provided to physicians working the service.
-
As the program is simultaneously covering all of the pilot communities (Langley, South Okanagan Similkameen, South Island, Thompson Region, and Victoria), it is likely that you will receive calls from outside your local area. You will have access to community overviews and lists of resources such as hours for the nearest emergency department, location of nearby after-hours pharmacies, etc. However, as the service focuses on semi-urgent and urgent issues, many of the connections to services that you would make during a clinic day won’t be required after hours.
Patient encounters
-
During the pilot, patient encounters will be via telephone calls, which are the most common and available technology. Due to the short time frame, the pilot is designed to be low-barrier for quick implementation. The HEiDi service found that a phone call is sufficient most of the time, and the service only uses Zoom occasionally for video calls with patients. We're looking into adding video capability to support physicians on shift for times when they determine it's needed for the patient visit.
-
FPSC's After Hours Care Program service is not set up to provide crisis or other types of counselling. Patients will be redirected as appropriate to crisis lines, other provincial/community mental health supports, or to follow up with their family physician. If medication advice is required, a patient call may be connected with a pharmacist or to the After Hours Care Program family physician as appropriate.
-
The service is organized to ensure that patient calls can be quickly answered, regardless of when they call during the service hours. During the pilot, we will gather data about the number of calls to expect at various times and days, and we will adjust the number of simultaneous staff accordingly—so that a physician only handles a reasonable number of calls (anticipated to be 3–5 per hour). If volume exceeds this, then additional physicians will be added. If there are times when there are no calls, then there may be labs or other items ordered by the service to review and identify appropriate management for.
-
During the pilot, the service could cover up to 550,000 attached patients; we expect that even at 2:00 a.m. there will be calls.
Patient charts
-
While currently there isn't the ability to access a patient’s cumulative health record from community, physicians working the After Hours Care Program service will have access to CareConnect and PharmaNet—more than many on-call doctors currently have. Following a patient encounter, the service will send the encounter note from the call via fax to the patient's community longitudinal family physician or nurse practitioner.
-
The patient chart is owned by HealthLink BC, which has responsibility of keeping records as per the requirements of the College of Physicians and Surgeons of British Columbia. The patient's MRP (most responsible provider) will also have a copy of the encounter note for the patient chart. Should an issue arise and the physician who provided care requires access to a chart in the future, that will be made available.
-
If the After Hours Care Program triage nurse is able to manage the issue, or sends the patient directly to ER, there will not be an encounter note sent to the patient's MRP. While this had been our original goal, the technical implementation of this is still in development and won't be available during the pilot.
Semi-urgent issues
-
When the physician staffing the service deems a patient’s issue to require attention from you within 3 business days, you will be contacted via a phone call to your mobile number. This call will be made by a physician staffing the service the morning following your patient’s call to the service, most likely between 8:00 a.m. and 9:00 a.m..
-
If the physician from the service is unable to reach you, they will attempt to reach your office to determine how bets to reach you/speak with your locum/colleague or medical director. If they are unable to reach you, then they may direct the patient to go to the ER, a local walk-in clinic, or UPCC.
Unattached patients
-
The pilot is for attached patients only. If the service expands, then we will explore providing services to unattached patients.
-
There are several ways the service will determine if a patient is attached:
-
HealthLink BC will provide a dedicated number for this service that's different from 811.
-
During the pilot, patients will be asked for the name of their clinic/family physician to confirm that they are attached. Ultimately, however, we will have to trust patients during the pilot. Should the service be deluged with calls, we will revisit this process. The roll out of the provincial attachment management system is expected to occur in late October; at this point, a patient's family physician/ nurse practitioner would easily be determined.
-
